Performance of Prognostic Heart FailureModels in Patients With NonischemicCardiomyopathy UndergoingVentricular Tachycardia Ablation
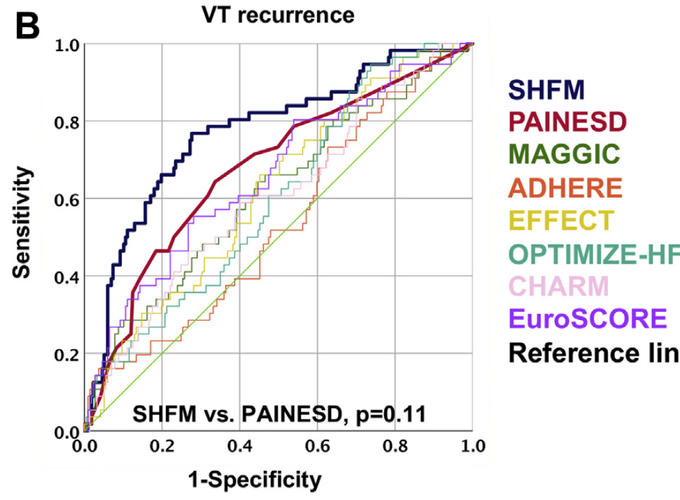 Receiver-operating characteristic (ROC) curves comparing the areas under the curve (AUC) of risk scores for death/transplant (A) and ventricular tachycardia (VT) recurrence (B).
Receiver-operating characteristic (ROC) curves comparing the areas under the curve (AUC) of risk scores for death/transplant (A) and ventricular tachycardia (VT) recurrence (B).
Performance of Prognostic Heart FailureModels in Patients With NonischemicCardiomyopathy UndergoingVentricular Tachycardia Ablation
Abstract
Objectives This study sought to assess the performance of established risk models in predicting outcomes after catheter ablation (CA) in patients with nonischemic dilated cardiomyopathy (NIDCM) and ventricular tachycardia (VT). Background A correct pre-procedural risk stratification of patients with NIDCM and VT undergoing CA is crucial. The performance of different pre-procedural risk stratification approaches to predict outcomes of CA of VT in patients with NIDCM is unknown. Methods The study compared the performance of 8 prognostic scores (SHFM [Seattle Heart Failure Model], MAGGIC [Meta-analysis Global Group in Chronic Heart Failure], ADHERE [Acute Decompensated Heart Failure National Registry], EFFECT [Enhanced Feedback for Effective Cardiac Treatment-Heart Failure], OPTIMIZE-HF [Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure], CHARM [Candesartan in Heart Failure-Assessment of Reduction in Mortality], EuroSCORE [European System for Cardiac Operative Risk Evaluation], and PAINESD [Chronic Obstructive Pulmonary Disease, Age > 60 Years, Ischemic Cardiomyopathy, New York Heart Association Functional Class III or IV, Ejection Fraction <25%, Presentation With VT Storm, Diabetes Mellitus]) for the endpoints of death/cardiac transplantation and VT recurrence in 282 consecutive patients (age 59 ± 15 years, left ventricular ejection fraction: 36 ± 13%) with NIDCM undergoing CA of VT. Discrimination and calibration of each model were evaluated through area under the curve (AUC) of receiver-operating characteristic curve and goodness-of-fit test. Results After a median follow-up of 48 (interquartile range: 19–67) months, 43 patients (15%) died, 24 (9%) underwent heart transplantation, and 58 (21%) experienced VT recurrence. The prognostic accuracy of SHFM (AUC = 0.89; goodness-of-fit p = 0.68 for death/transplant and AUC = 0.77; goodness-of-fit p = 0.16 for VT recurrence) and PAINESD (AUC = 0.83; goodness-of-fit p = 0.24 for death/transplant and AUC = 0.68; goodness-of-fit p = 0.58 for VT recurrence) were significantly superior to that of other scores. Conclusions In patients with NIDCM and VT undergoing CA, the SHFM and PAINESD risk scores are powerful predictors of recurrent VT and death/transplant during follow-up, with similar performance and significantly superior to other scores. A pre-procedural calculation of the SHFM and PAINESD can be useful to predict outcomes.